Semaglutide helps type 1 diabetes
Semaglutide Shows Promise in Type 1 Diabetes Management A Potential Breakthrough in Treatment
In a groundbreaking development that could redefine the future of diabetes care, recent clinical trials have indicated that the drug semaglutide originally approved for treating type 2 diabetes and obesity may offer significant benefits for individuals with type 1 diabetes. Long considered an autoimmune condition requiring lifelong insulin dependency, type 1 diabetes has traditionally had limited pharmacological treatment options beyond insulin therapy. However, emerging evidence suggests that semaglutide may help improve glycemic control, reduce insulin requirements, and even slow down the progression of beta cell failure in type 1 patients. These findings are sparking renewed hope among patients, caregivers, and researchers in the global diabetes community.
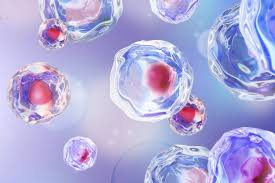
Semaglutide is a glucagon like peptide 1 (GLP 1) receptor agonist. It mimics the natural hormone GLP 1, which helps regulate blood sugar by enhancing insulin secretion, suppressing glucagon production, slowing gastric emptying, and promoting satiety. These mechanisms make semaglutide effective in type 2 diabetes, where insulin resistance is the central issue. However, type 1 diabetes is marked by the autoimmune destruction of insulin producing beta cells in the pancreas. Until recently, it was believed that GLP 1 analogues would have little to no impact in type 1 patients, who typically produce little to no endogenous insulin. That assumption is now being challenged by new data.
Several clinical studies, including small scale randomized controlled trials and pilot observational research, have demonstrated that type 1 patients treated with semaglutide experience notable benefits. One such study, conducted across multiple diabetes centers in Europe and North America, found that participants on semaglutide therapy required 20 30% less insulin while maintaining stable or improved HbA1c levels. Moreover, these patients reported reduced glycemic variability a significant factor in preventing complications such as retinopathy, neuropathy, and cardiovascular disease. Another study noted that patients using continuous glucose monitors (CGMs) while on semaglutide had longer durations within the target glucose range, a critical marker of daily glycemic control.
What makes these findings even more compelling is that semaglutide also appears to aid in weight management among type 1 diabetes patients many of whom struggle with weight gain due to intensive insulin therapy. Insulin promotes fat storage, and over time, patients who must use high doses may experience increased abdominal fat, raising the risk of insulin resistance and heart disease. Semaglutide’s appetite suppressing and weight reducing properties offer a two fold benefit improved metabolic health and potential psychological relief from the burden of diabetes related weight gain. In clinical settings, patients have reported losing between 5 to 12 percent of their body weight after six months of adjunct semaglutide therapy.
It is important to note, however, that semaglutide is not a cure for type 1 diabetes. Insulin therapy remains essential, as semaglutide does not replace the hormone that type 1 patients lack. Instead, it acts as an adjunct therapy that may reduce the amount of insulin needed and smooth out the daily fluctuations in blood glucose levels that make diabetes management so difficult. Experts caution that semaglutide should be used under strict medical supervision, particularly given its potential side effects, such as nausea, vomiting, delayed gastric emptying, and in rare cases, pancreatitis. Nonetheless, the potential to improve quality of life and long term outcomes is generating excitement.
From a scientific standpoint, the mechanism by which semaglutide benefits type 1 diabetes patients is still being explored. One hypothesis is that even in individuals with type 1 diabetes, some residual beta cell function remains for years after diagnosis. Semaglutide may enhance this residual activity or protect surviving cells from further autoimmune destruction. Additionally, its ability to suppress post meal glucagon spikes which can contribute to hyperglycemia in type 1 patients is believed to play a major role. By blunting the release of glucagon and delaying gastric emptying, semaglutide may create a more stable postprandial glucose profile, thereby reducing the need for corrective insulin doses.
These promising results are already prompting pharmaceutical companies and research institutions to expand trials. Phase 3 studies with larger, more diverse patient populations are underway to confirm efficacy, safety, and optimal dosing protocols for semaglutide as an adjunct in type 1 diabetes. Regulatory bodies such as the U.S. FDA and European Medicines Agency are closely monitoring these studies. If the outcomes are favorable, it is likely that semaglutide could receive approval for use in type 1 diabetes within the next few years, dramatically altering the treatment landscape. Endocrinologists are cautiously optimistic, seeing the drug as a potential game changer for patients who experience poor glycemic control despite rigorous insulin regimens.
For the millions of people around the world living with type 1 diabetes, the implications of this research are profound. Managing type 1 diabetes is a 24/7 challenge, involving constant monitoring, insulin injections or pump adjustments, dietary vigilance, and the ever present risk of hypoglycemia. The addition of semaglutide to the treatment arsenal could offer patients a greater sense of stability, reduce burnout, and minimize complications that arise from glucose fluctuations. Patient advocacy groups have already begun pushing for expanded access to semaglutide trials and educational campaigns to ensure that people are informed about this emerging option.
In conclusion, semaglutide’s potential to aid in the management of type 1 diabetes marks a significant advancement in the field of endocrinology. While much research remains to be done to understand its long term safety and effectiveness, early results are highly encouraging. As new therapies emerge and existing ones find novel applications, the future of diabetes care is becoming increasingly personalized, integrated, and hopeful. Semaglutide may not replace insulin, but it represents an important stride toward more effective, manageable, and compassionate treatment for those living with type 1 diabetes.